Gastrointestinal Physiology
Describe the progress of a simple meal through the gastrointestinal tract. This meal consists of dipeptides (mixed amino acid composition), sucrose, and triglycerides. Include key points in processing that alter the chemical form of these nutrients and result in their appearance in the blood stream, as well as events that aid their flow. Your answer can be in the form of an essay or detailed outline. Include diagrams that would aid the explanation.
Mouth
Mechanical Digestion: Chewing breaks down food into smaller particles, increasing the surface area for enzymatic action.
Chemical Digestion :
Carbohydrates: Salivary amylase begins the digestion of starches but has minimal effect on sucrose.
Lipids and Proteins: No significant digestion occurs for triglycerides or dipeptides in the mouth.
Esophagus
Transports the bolus ( chewed food ) to the stomach via peristaltic movements without significant digestion.
Stomach
Mechanical Digestion: Churning mixes the food with gastric juices to form chyme.
Chemical Digestion :
Proteins/Dipeptides :
Pepsinogen is activated to pepsin in the acidic environment ( pH ~2 ) , breaking down proteins into smaller peptides.
Dipeptides may be further cleaved into amino acids.
Lipids :
Gastric lipase initiates the breakdown of triglycerides into diglycerides and free fatty acids.
Carbohydrates: Limited digestion of sucrose occurs here.
Small Intestine
Duodenum :
Pancreatic Enzymes :
Pancreatic Lipase: Continues triglyceride digestion into monoglycerides and free fatty acids.
Proteases (Trypsin, Chymotrypsin, Carboxypeptidase): Further break down peptides into amino acids and dipeptides.
Pancreatic Amylase: Acts on any remaining starches.
Bile Salts :
Emulsify fats to form micelles, enhancing lipid digestion and absorption.
Jejunum :
Brush Border Enzymes :
Sucrase: Hydrolyzes sucrose into glucose and fructose.
Peptidases: Split dipeptides into free amino acids.
Absorption :
Monosaccharides :
Glucose and Galactose: Absorbed via SGLT1 ( sodium-dependent glucose transporter ).
Fructose: Absorbed via GLUT5 transporter.
Amino Acids :
Absorbed through various sodium-dependent amino acid transporters.
Lipids :
Micelles deliver monoglycerides and fatty acids to enterocytes.
Inside enterocytes, re-esterified into triglycerides.
Packaged into chylomicrons for lymphatic transport.
Ileum :
Continues absorption of nutrients and bile salts.
Large Intestine
Absorption: Reabsorbs water and electrolytes.
Microbial Fermentation: Further breaks down undigested carbohydrates.
Entry into the Bloodstream
Amino Acids and Monosaccharides :
Enter capillaries in the villi.
Transported to the liver via the hepatic portal vein.
Lipids :
Chylomicrons enter the lymphatic system through lacteals.
Eventually enter the bloodstream via the thoracic duct.
Events Aiding Flow
Peristalsis: Smooth muscle contractions propel food through the GI tract.
Segmentation: Mixes chyme to enhance nutrient absorption.
Hormonal Regulation :
Gastrin: Stimulates gastric acid secretion.
Secretin: Promotes bicarbonate secretion from the pancreas.
Cholecystokinin (CCK): Stimulates bile and pancreatic enzyme release.
Neural Regulation :
Enteric Nervous System: Coordinates digestion and absorption processes.
Consider the steady-state of an epithelium actively absorbing glucose by the electrogenic mechanism using 2Na+ \ glucose-cotransporters.
Intracellular concentrations are : 13 mM glucose , 16 mM Na , 156 mM K+ , 37 mM CI
Luminal concentrations are : 7 mM glucose , 145 mM Na , 5 mM K+ , 106 mM CI
Interstitial concentrations are : 5 mM glucose , 145 mM Na , 5 mM K+ , 106 mM Cl
The Nernst potentials ( Eion ) are : ENa = +59 mV , EK = -92 mV , ECl = -28 mV
The basolateral membrane electrical potential difference ( Vb ) is 63 mV , cell-side negative with respect to extracellular. The transepithelial electrical potential difference ( Vte ) is 19 mV , lumen negative with respect to the interstitial space. Answer the following questions concerning this epithelium; include diagrams that would aid the explanation.
a.) During this steady-state absorption, what is the glucose conductance of the apical membrane uptake compared to the glucose conductance of the basolateral membrane exit?
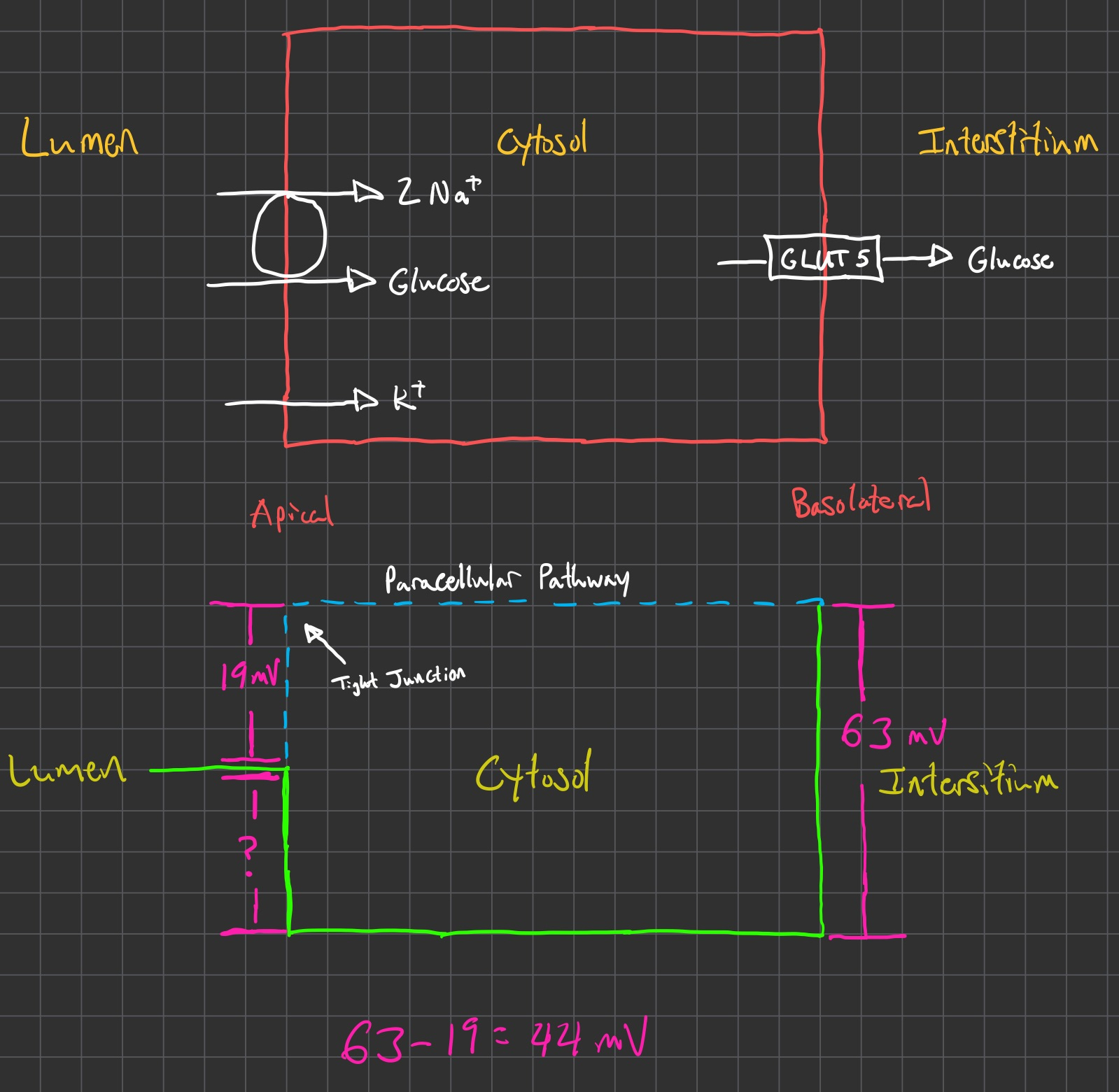
Apical Side
Voltage ( mV ) Charge ( z ) Population ( n ) Total Voltage ( mV ) Driving Force ( mV ) Direction -16.13 Neutral ( 0 ) 1 In +57.43 +1 2 In +44 N / A N / A N / A N / A Net In Basolateral Side
Voltage ( mV ) Charge ( z ) Population ( n ) Total Voltage ( mV ) Driving Force ( mV ) Direction -24.90 Neutral ( 0 ) 1 Out +63 N / A N / A 0 N / A N / A Net In Comparison
we can replace resistance
now , rewrite it , in terms of current
the normal for the driving force is :
but he says just to sum up all of the voltages on apical and basolateral side and treat this as the "driving force"
For the comparison though , we will just write 2 of these Ohm's law equations.
1 for for the apical side , and 1 for the basolateral side
and then divide 1 by the other
also , because we are in "steady-state" , aka the same amount of glucose that is absorbed is also secreted
then we can set the "current" or "flow" or
for example , say 6 glucose molecules flow through apical membrane
then 6 also flow out through basolateral membrane
6/6 or whatever we choose will reduce to 1/1
Apical Membrane :
Glucose uptake via 2Na+ / glucose cotransporter ( SGLT1 )
Active transport against glucose gradient ( from 7 mM in lumen to 13 mM intracellularly )
Low conductance due to dependence on Na+ gradient and carrier saturation
Basolateral Membrane:
Glucose exit via facilitated diffusion through GLUT transporter.
Passive transport down glucose gradient ( from 13 mM intracellularly to 5 mM interstitially )
Higher conductance due to passive diffusion and continuous gradient.
The glucose conductance of the apical membrane is lower compared to the basolateral membrane. The active transport mechanism on the apical side limits conductance, whereas the basolateral side allows for higher conductance due to passive diffusion.
b.) Opening apical membrane K+ channels will result in transepithelial K+ secretion.
Assume the same electrical potential differences and Nernst potentials ( Eion ) as above. If net flow of K+ through the basolateral membrane K+ channels is 5 times greater than the net K+ flow through the apical membrane K+ channels , then how large is the apical membrane K+ conductance compared with the basolateral membrane K+ conductance?
Apical
Voltage ( mV ) Charge ( z ) Population ( n ) Total Voltage ( mV ) Direction -89.65 +1 1 Out +44 N / A N / A +44 In Net Out Basolateral
Voltage ( mV ) Charge ( z ) Population ( n ) Total Voltage ( mV ) Direction -89.65 +1 1 Out +63 N / A N / A +63 In Net Out The apical membrane K+ conductance is approximately 11.67% of the basolateral membrane K+ conductance.
Alternatively , the basolateral membrane K+ conductance is 8.56 times larger than the apical membrane K+ conductance.
c.) If luminal K+ concentration increases as a result of K+ secretion ( assuming the same electrical potential differences ) , then net K+ flow through the apical membrane K+ channels would stop at what value for the K+ Nernst potential at the apical membrane, EK?
What luminal K* concentration would occur when net flow of K+ stops, through these apical membrane K+ channels?
Voltage ( mV ) Charge ( z ) Population ( n ) Total Voltage ( mV ) Direction ? +1 1 Out +44 N / A N / A +44 In Net 0 In Ok , now we setup the nernst to solve for our missing concentration in the lumen :
Renal Physiology
During a routine wellness visit, your physician informed you, with a concerned look, that your extracellular fluid volume was 13 L. Since you had just completed a course in human physiology, you immediately began calculating in your head what your ECE volume likely had been previously.
If your body weight had been 60 kg until recently, how much had your extracellular fluid volume changed compared with your previous healthier steady-state value?
60 kg is average female
A healthy individual has clinical lab values for creatinine concentration and urine flow rate :
Pcr = 81 µM , Ucr = 3.3 mM , UFR = 2.8 mL/min. What was their glomerular filtration rate?
A healthy individual has clinical lab values for creatinine concentration and urine flow rate: Pcr = 62 µM , Ucr = 6.6 mM , UFR = 1.2 mL/min. What was their daily production rate of creatinine?
A healthy individual has the following clinical lab values: Pcr = 98 µM , Ucr = 1.5 mM , UFR = 8.3 mL/min. What was their fractional excretion of water ( FEwater ) ?
Fractional Na* excretion ( FENa ) is the Na+ excretion rate as a proportion of the Na+ filtered rate. What is the fractional excretion of Na+ for the condition when : Pcr = 78 µM , Ucr = 1.4 mM , PNa = 146 mM , UNa = 18 mM ?
Glomeruli in the kidney are the sites of blood filtration, which is the first step in urine formation. ( Drawing a diagram showing the arrangement of a glomerulus with its associated arterioles may help in your explanations. )
a.) Explain how blood pressure will change in the glomerular capillaries and in the peritubular capillaries during a moderate constriction of the efferent arterioles?
In moderate efferent arteriole constriction:
In the glomerular capillaries: Blood pressure will increase because the exit pathway for blood is more constricted, leading to a backup of pressure in the glomerulus.
In the peritubular capillaries: The pressure will decrease because less blood flow will be reaching this area post-constriction.
b.) Explain how glomerular filtration rate will change during this moderate efferent constriction?
A moderate efferent arteriole constriction generally increases GFR initially due to the increased glomerular capillary hydrostatic pressure, which enhances filtration. However, excessive constriction could reduce GFR by severely limiting blood flow.
The renal proximal tubule contributes to systemic acid/base balance by reabsorbing
which promotes the conversion of
Thus, the presence of
indirectly increasing the
A renal tubule segment in the outer medulla is the thick ascending limb of Henle's loop. Explain how these cells produce transepithelial Cl- absorption and associated K+ secretion. Also, explain how these events influence the flow of at least two other solutes across this tubular epithelium, including the direction of net flow and permeability routes for each. ( Drawing a diagram of a thick ascending limb cell showing the key transport steps in the apical and basolateral membranes may aid in your explanation of transepithelial solute flow. )
In the thick ascending limb of Henle’s loop:
Cl absorption occurs via the Na-K-2Cl cotransporter on the apical membrane, bringing these ions into the cell.
K secretion is facilitated through K+ channels back into the lumen to maintain electrical neutrality.
his transport results in a positive lumen potential, promoting:
Na reabsorption paracellularly into the interstitial fluid.
Ca and
Two patients have a series of renal lab tests performed, and incidentally one is in diuresis (Patient A) and the other is in anti-diuresis (Patient B). Unfortunately, you receive only the last page of the report (without patient identifiers) that includes the tubular fluid osmolarities at the end of the thick ascending limb and at the end of the distal tubule (see below).
| sample 1 | sample 2 | |
|---|---|---|
| end, thick ascending limb | 97 mOsm | 102 mOsm |
| end, distal tubule | 293 mOsm | 92 mOsm |
a.) Match the samples to the 2 patients.
Patient A = Diuresis = Sample 2
Patient B = Anti Diuresis = Sample 1
b.) Explain the renal physio-logic that you will use to convince your colleagues that your interpretation is correct. Include a diagram if that will aid in your explanation.
There is a high concentration of osmoles left in distal tubule in Sample 1
This means water was re-absorbed and not urinated out ( anti-diuresis )
The distal renal tubule includes 2 distinct cell types adjacent to each other in the epithelium, principal cells ( apical membrane Na+ channels and K+ channels ) and intercalated cells ( apical membrane H+ pumps ). ( Drawing a diagram for each cell type showing the key transport steps in the apical and basolateral membranes may aid in your explanation of the transepithelial solute flow. )
a.) For a person with high diet in K+ , what hormonal response will act to maintain whole body K+ balance ?
Aldosterone Secretion: High plasma K+ levels stimulate the adrenal cortex to release aldosterone, which acts primarily on the distal renal tubule and the collecting ducts in the kidney.
Effect of Aldosterone: It increases the activity of certain channels and pumps in the renal tubular cells to promote potassium excretion and sodium reabsorption, helping to balance potassium levels in the body.
b.) How does this hormone alter the activity of these 2 cell types ?
Principal Cells:
Apical Membrane Na+ and K+ Channels: Aldosterone increases the number and activity of epithelial sodium channels ( ENaC ) and potassium channels ( ROMK ) on the apical membrane of principal cells.
Basolateral Na-K-ATPase Pump: Aldosterone also upregulates the Na-K-ATPase on the basolateral membrane, which pumps sodium into the blood and potassium into the cell.
Overall Effect: With more active sodium channels, sodium is reabsorbed from the tubular lumen, creating a negative charge in the lumen that promotes potassium secretion. This increases potassium excretion in the urine, aiding in the regulation of potassium levels.
Intercalated Cells:
Apical Membrane H+ Pumps: While aldosterone primarily affects principal cells for potassium balance, intercalated cells can also respond indirectly. Increased sodium reabsorption in the principal cells drives a gradient that promotes proton ( H+ ) secretion in intercalated cells to help balance charge.
Potassium Reabsorption ( Type A Intercalated Cells ): In some cases, type A intercalated cells can reabsorb potassium via a K-H exchanger, especially in low potassium states. However, in high potassium conditions, aldosterone mainly enhances potassium excretion by acting on principal cells.
Adaptation to living at high altitude requires changes in your renal function.
a.) What is the stimulus that leads to the altered renal function?
Hypoxia ( low oxygen availability )
Leads to Alkalosis , due to breathing off excess CO2
b.) Which segments of the renal tubule respond with major changes in transepithelial flow?
Proximal Tubule = secretes / retains more bicarbonate
Collecting Duct = reduced ADH = reduced water reabsorption
c.) Which plasma solute changes in concentration most dramatically?
HCO3-
d.) What consequence of renal compensation likely requires your conscious intervention?
Dehydration = need fluid replenishment
e.) What renal change will occur upon your return to sea level ( low altitude ) ?
Decrease bicarbonate excretion
Switch back to re-absorbing bicarbonate at a normal amount